The Emergency Care Competence Needed for Police Patrol Officers According to the Experts
– a National Swedish Delphi Study
RN, PEN, MNSc (Lecturer), PhD student, Centre of Interprofessional Cooperation within Emergency care (CICE), Faculty of Health and Life sciences, Linnaeus University, Department of Ambulance Service, Region Kronoberg, Växjö, Sweden
Corresponding author
RN, PEN, PhD, Associate Professor, Centre of Interprofessional Cooperation within Emergency care (CICE), Faculty of Health and Life sciences, Linnaeus University, Växjö, Sweden, Department of Ambulance Service, Region Sörmland, Katrineholm and Centre for Clinical Research Sörmland, Uppsala University, Eskilstuna, Sweden
RN, PhD, Associate Professor, Centre of Interprofessional Cooperation within Emergency care (CICE), Faculty of Health and Life sciences, Linnaeus University, Växjö and Centre for Prehospital Research (PreHospen), Faculty of Caring Science, Work Life and Social Welfare, University of Borås, Sweden
PPO, PhD, Assistant Professor, Centre of Interprofessional Cooperation within Emergency care (CICE), Department of Police Work, Faculty of Social Sciences, Centre for Police Research and Development, Linnaeus University, Växjö, Sweden
RN, PEN, PhD, Assistant Professor, Centre of Interprofessional Cooperation within Emergency care (CICE), Faculty of Health and Life sciences, Linnaeus University, Department of Ambulance Service, Region Kronoberg, Växjö, Sweden
Publisert 16.06.2022, Nordic Journal of Studies in Policing 2022/1, side 1-15
Police patrol officers (PPOs) face different types of encounters with acutely ill and injured people as first responders. The study aim was to explore and describe the emergency care competence needed for Swedish PPOs. The study had an exploratory design, and the data was collected using the Delphi technique from 43 experts in Sweden: police program educators (n=10), police authority instructors (n=11), and PPOs (n= 22). The results generated an understanding of emergency care competence that is relevant for PPOs. Basic assessment and basic life support measures for traumatic injuries and cardiac arrest (e.g., airway management, cardiopulmonary resuscitation (CPR), and hemorrhage control) received the highest levels of agreement among the experts, whereas more advanced assessments (taking care of people suffering from mental/medical illness or with drug/alcohol abuse) received lower levels of agreement. These results provide support for educators at the police programs and for the police authority in preparing PPOs to perform relevant out-of-hospital emergency care.
Keywords
- Competence
- Delphi technique
- education
- first responder
- police patrol officers
- prehospital emergency care
1. Introduction
Police patrol officers (PPOs) face multifaceted, everyday challenges that demand professionals capable of adapting to a wide range of situations and decisions. One of their most important societal functions is to protect and save lives, and PPOs may on many occasions be the first authority at a scene in out-of-hospital emergencies (Hawkins et al., 2007; Klassen et al., 2018). A study from the United States (US) covering 41 states in 2014 indicates that assignments where PPOs deliver care prior to the arrival of the ambulance service mostly concern cardiac arrest and traumatic events (Klassen et al., 2018). Other findings in studies from the US also indicate that PPOs face challenges in a wide range of situations involving medical and mental health related complaints and emergencies (Hawkins et al., 2007; Rosen & Travers, 2021). Being first on the scene as a first responder may be chaotic and frightening, while awaiting the ambulance service creates feelings of loneliness in a perceived eternity. However, having had training in a systematic way of providing emergency care creates feelings of security in these chaotic situations (Elmqvist et al., 2010). The emergency care training and equipment provided for PPOs to act as first responders varies between different countries (Dekanoidze, 2018; Hawkins et al., 2007). Despite these variations, PPOs worldwide face a somewhat similar type of challenge when awaiting the arrival of emergency medical support or when transporting acutely ill or injured persons to health care facilities. Earlier research from the US indicates that PPOs themselves support the call for additional training in emergency care (Alonso-Serra et al., 1997) and a need to develop police-specific emergency care training has been emphasized (Sztajnkrycer et al., 2007). Furthermore, calls have also been made for a better understanding of the challenges PPOs face concerning emergency care in order to develop their training and policy recommendations (Klassen et al., 2018). There is little research from a European perspective and none at all from a Swedish perspective.
1.1 Background
The design and content of the educational program for PPOs and their pathways for gaining employment vary in European and westernized countries (Dekanoidze, 2018). A 2.5-year post-secondary school program for PPOs is offered at five different Swedish universities in collaboration with the National Swedish Police Authority (2021). The police authority provides a national curriculum for the program, which forms the basis for each university’s own syllabus. There are several general points in the curriculum with relevance for emergency care, but none of them are specific. This is not unique as university curriculums in Sweden normally consist of general formulations targeting different aspects of competence (Knowledge and understanding, Skills and abilities, Evaluation abilities and approach), which translate into the content for professional programs. Police work is defined in the present curriculum (National Swedish Police Authority, 2020) as an interdisciplinary field of several relevant topics, such as criminology, law, emergency care, behavioral science, social work, and political science (SOU 2016:39; SOU 2008:39). However, with no additional definitions of what constitutes emergency care for PPOs, there is thus room for interpretation when syllabuses are developed at each police program. The syllabuses covering emergency care in the five Swedish universities focus generally on four main areas: (i) Basic life support measures in cases of illness; (ii) Identification and proper management of diseases/conditions that may be confused with symptoms of drug or alcohol abuse, where inadequate assessment might result in an acutely ill person ending up in police custody without relevant medical attention (FAP 023-1); (iii) Basic life support measures in cases of injury (FAP 776:1); and (iv) Emergency care of people with mental illness. The first three main areas are often implemented in courses led by educators with backgrounds in emergency care and clinical experiences from the ambulance service or emergency department. The fourth has traditionally been implemented in a separate syllabus in the police program and is led by educators with mental health and/or behavioral science backgrounds. The PPOs must also manage an initial criminal investigation in several of these situations and/or manage a situation with potential danger to public order and safety. This contextual condition highlights the necessity of topical integration in each educational situation, which has also been defined as a general target in the curriculum. Local deviations occur between different police programs in terms of allocated time, educational strategies, and specific content for emergency care competence. For example, anatomy is defined separately in some of the police program syllabuses and the prevention of infection in others. Some police programs disperse the emergency care course content throughout all semesters, while other police programs complete the course during one or two semesters. All universities in Sweden implement a six-month internship at the end of the police program where the students work with two active PPOs prior to graduation and employment. There are no points regarding competence in emergency care in the assessment form used to evaluate the students’ performance during the internship.
The Swedish Police Authority is organized into seven geographical regions and nine national departments. There is annual complementary training for active PPOs in Polkon (Police Conflict Management), which mainly consists of arms training, tactical training, and occasionally emergency care focusing on injuries caused by the actual violence applied by the police (FAP 776:1). The police authority equips each patrol car with a standardized emergency care equipment bag, and some police districts are equipped with automated external defibrillators (AED). The contents of this emergency care equipment bag mirror the police authority’s expectations as to which kind of emergency care needs every PPO might face and therefore need to master (FAP 023-1; FAP 776:1). There are, however, no national guidelines stipulating the content or scope of the complementary training, nor a specified certificate in emergency care required for PPOs, even though several initiatives have been taken to include such an annual defined mandatory training. The conditions and allocated time for the instructors responsible for education may thus differ greatly, and a detailed overview of the complementary training and competence in emergency care for Swedish PPOs has not been documented by the police authority.
There are several reasons as to why PPOs are faced with situations concerning acutely ill and injured persons. One is that PPOs may be the first on the scene to initiate lifesaving actions (Band et al., 2014; Kooij et al., 2004). Another is that PPOs are taking care of people with mental illness or assigned to transfer people to a hospital for continued psychiatric care (Erdner & Piskator, 2013). According to Swedish legislation (FAP 023-1), PPOs are also responsible for assessing and making decisions as to whether people with impacted consciousness levels, suspected to be related to alcohol/drug use, should be taken into police custody or need further medical attention. PPOs, thus, need different competencies to provide for several different needs when faced with acutely ill and injured persons.
Competence can be described as the individual’s capability to cope with certain situations in a successful way so that best practice quality and standards are maintained (Ellström, 1997). Competence also entails integrating and using both theoretical and practical knowledge (Eraut, 1998). However, PPOs emergency care competence must be understood in a complex context where decisions and activities are prioritized and carried out in relation to other tasks of the police service. The competence considered necessary for PPOs is influenced by, e.g., professional organizations, institutions of higher education, and governmental agencies (Eraut, 1998). There are no formal Swedish national requirements or detailed descriptions which stipulate necessary emergency care competence for PPOs. Basic information on the total number of the various types of police assignments related to emergency care is available in the Police Authority’s databases for the years up to 2020, but no further detailed data is accessible in these sources (Polisen.se, 2020). There are no studies evaluating the educational interventions applied in order to support PPOs in coping with situations involving emergency care needs. In summary, there is a lack of clarity, and a need for a greater understanding, of relevant emergency care competence for PPOs. The aim of this study was, thus, to explore and describe the emergency care competence needed for Swedish PPOs.
2. Methods
An exploratory design was adopted using a Delphi technique (Keeney et al., 2011).
2.1 Study setting and participants
A group of experts is selected for a study where the Delphi technique is to be used, in which an expert is assessed as someone with greater knowledge of the topic under investigation than others have (Keeney et al., 2011). The study was conducted in Sweden including participants from all five universities offering the police program and all seven police regions (Table 1). Initially, the first author contacted the head of the police program at each university and asked for contact information for two of their most experienced educators in emergency care. Two to three experts were identified from each of the five police programs, and all were invited to participate (n=11). The first author then contacted the National Head of Instructors in the Swedish Police Authority and requested contact information for all head instructors in each of the seven police regions. Some regions had more than one head instructor, and all were invited to participate (n=11). Subsequently, the head instructors were asked to identify two of the most experienced PPOs in their region – preferably one from a rural area and one from a metropolitan area. The number of proposed experienced PPOs varied between fewer than two to more than two from each region, but they were all invited to participate in the study (n=23). All 45 invited participants agreed to take part in the study. However, two experts (one educator from the police program and one PPO) withdrew their consent to participate via e-mail prior to Round 1 due to changed working conditions. A total of 43 experts thus participated: educators at the police programs (n=10), instructors in the Police Authority (n=11), and active PPOs (n= 22).
| Total number of experts | 43 |
| Educators in the police program | 10 |
| Instructors in the Police Authority | 11 |
| Active police patrol officers | 22 |
| Numbers of experts from each police region | |
| A | 7 |
| B | 6 |
| C | 5 |
| D | 9 |
| E | 9 |
| F | 4 |
| G | 3 |
| Years of experience | |
| Educators in the police program | Range 1–20Mean 6.1SD 7.0 |
| Instructors in the Police Authority | Range 4–16 Mean 11.8SD 4.1 |
| Active police patrol officers | Range 1–32 Mean 9.1SD 6.8 |
2.1.1 The experts
The experience of the Educators in the police program ranged between 1 and 20 years (mean 6.1). Most of them also had several years of experience as a registered nurse (RN) and specialist training within emergency care. A majority were specialist-trained RNs within ambulance care and still clinically active part-time. The experience of the Instructors in the Police Authority ranged between 4 and 16 years (mean 12.7). All the instructors, except for one, had several years’ experience as a PPO, and most of them were still active. Two thirds had additional training, education, and/or experience in emergency care from the fire department, the army, and/or the ambulance service. The experience of the Active PPOs ranged between 1 and 32 years (mean 9.6). Two thirds of the active PPOs had some form of additional training, education, and/or experience in emergency care from the fire department, the army, and/or the ambulance service.
2.2 Data collection
The data were collected in four Rounds during October and November in 2020.
2.2.1 Round 1
In Round 1, an e-mail with an open-ended question was sent to all the experts: “What does a Swedish Police patrol officer need to know in order to help acutely ill or injured persons?” All the experts (n=43) answered the e-mail. The first and last authors read through all e-mails and extracted areas expressing necessary emergency care competence for Swedish PPOs. These areas were then reformulated for clarification and compared with each other to reduce redundancy. All authors participated in critical discussions regarding the extraction of areas and the clarification process. A total number of 76 areas of emergency care competence were extracted from the responses in Round 1. These areas underwent a test for face validity by a group of five experienced PPOs who were not participating in the study.
2.2.2 Round 2
The 76 areas were included in a questionnaire and sent to the experts in Round 2. The experts were asked in the questionnaire to rate to what extent they agreed with each area using a five-point Likert scale, ranging from (1) ‘not agree’ to (5) ‘strongly agree’. The scale was tricotomized to a three-point scale for analytical purposes prior to determining the level of consensus (Svensson et al., 2021). This resulted in expert ratings of 1–2 on the Likert scale for an item as corresponding to ‘not agree’, 3 corresponding to ‘neutral’ and 4–5 corresponding to ‘agree’. The consensus level was set at 75% prior to the data collection (Keeney et al., 2011). An area was thus considered to have achieved consensus when ≥ 75% of the experts agreed on any of the tricotomized scale responses. The questionnaire was distributed by SurveyMonkeyÒ individually to all experts from Round 1. Two reminders were sent by e-mail during the first 10 days and one reminder via cellular text message day 12, asking the experts to answer the questionnaire. The questionnaire in Round 2 was open for a total of 14 days. All the experts returned the questionnaire, resulting in a 100% response rate in Round 2. A total of 36 areas achieved consensus in Round 2. Furthermore, the experts were given the opportunity of adding areas of emergency competence in free text that they thought were missing in the questionnaire. These areas were then included in further rounds. This resulted in nine additional areas from Round 2 being added to the following questionnaire (Table 2).
| Round 1 | → | Round 2 | → | Round 3 | → | Round 4 | |
| Number of experts | 43 | 43 | 43 | 43 | |||
| Response rate | 100% | 100% | 100% | 100% | |||
| Drop-out | 0 | 0 | 0 | 0 | |||
| Round activity | E-mail with an open-ended question | → | Questionnaire with 76 areas | → | Questionnaire with 49 areas (40 not reaching consensus in Round 2 + 9 new) | → | Questionnaire with 36 areas (not reaching consensus in Round 3) |
| ÷ | ÷ | ÷ | |||||
| Items reaching consensus | 36 | 13 | 2 |
2.2.3 Round 3
In Round 3, a questionnaire was sent containing the areas where consensus had not been achieved in Round 2 together with the nine new areas that had emerged from the free text answers in Round 2. A total of 49 areas were included in the questionnaire and sent to the 43 experts in Round 3 (Table 2). Mean values of the responses from the experts’ answers in Round 2 were added to each item in the questionnaire in Round 3. The experts were encouraged to take the mean values into consideration while once again rating their level of agreement in the Likert scale. Two reminders were sent by e-mail during the first 10 days and one reminder via cellular text message on day 12, asking the experts to answer the questionnaire. The questionnaire in Round 3 was open for a total of 14 days. All the experts returned the questionnaire, resulting in a 100% response rate in Round 3. The experts were also given the opportunity to add areas of emergency care competence in free text that they thought were missing in the questionnaire, as previously done in Round 2. However, there were no areas that had not already been addressed which were suggested to be added to the questionnaire from Round 3.
2.2.4 Round 4
A third questionnaire was sent out containing areas where consensus had not been achieved in Round 3, resulting in 36 areas distributed to the 43 experts (Table 2). The mean values of the responses from the experts’ answers in the previous round were added to each area in the questionnaire in Round 4. The experts were encouraged take the mean values into consideration while once again rating their level of agreement in the Likert scale. Two reminders were sent by e-mail during the first 10 days and one reminder via cellular text message on day 12, asking the experts to answer the questionnaire. The questionnaire in Round 4 was open for a total of 14 days. Consensus was achieved for a further two areas in Round 4. Consensus had thus been achieved in a total of 51 (60%) of the 85 areas (the initial 76 from Round 2 together with the additional 9 from Round 3) included in the questionnaire. All the 43 included experts from Round 1 completed all four rounds.
2.3 Ethical considerations
The study followed the principles of the Declaration of Helsinki, and the Ethics Committee in the southeast of Sweden reviewed the study’s ethics and provided an advisory ethical statement prior to the study (No. 639-2020). Written consent to proceed with the study was procured from the heads of the police regions and the heads of the police programs. Written consent to participate was obtained from the participants when answering the e-mail in Round 1 and implied when answering the questionnaires in the consecutive three rounds. All participants were informed that they could withdraw their participation at any time and were ensured confidentiality.
3. Results
The results indicated that basic life support measures received the highest levels of agreement in terms of the necessary emergency care competence for Swedish PPOs (Table 3). The top ten areas, achieving an almost 100% level of agreement, represent abilities to perform CPR with AED (areas 1, 2 and 8), to stop massive hemorrhaging (areas 3, 4 and 10), and measures for basic airway management (areas 5 and 6), while simultaneously concerning working in a hazardous environment (areas 7 and 9). Many of the areas with the highest level of agreement are concerned with traumatic injuries (e.g., areas 3, 4, 7, 10 and 12) and the ability to assess and take care of these in a systematic way, using the S-CABCDE template as a support for doing so (area 14). When addressing more advanced assessments, and taking care of acutely ill people, the level of agreement was reduced (e.g., areas 20, 24, 35 and 43). The levels of agreement also indicate some uncertainties concerning the abilities to assess and care for people with mental illness (areas 39, 46 and 47), and people with alcohol and/or drug use (areas 41 and 48). Moreover, consensus was not achieved for four of these (areas 41, 46, 47 and 48) until Round 3. Furthermore, the results revealed some outliers such as performing CPR on adults (area 1) where all experts agreed (M=5, SD=0, R=5-5), whereas performing CPR on children (area 19) had (M=4,7, SD=0,77, R=1-5). There were also lower levels of agreement and a wide range (1–5) in terms of identification and evaluation of threats to life (areas 20 and 21) compared with the high levels of agreement concerning applying suitable measures for the aforementioned threats to life (areas 1–10), such as life-saving actions. There were also lower levels of agreement and a wide range concerning assessing respiration/consciousness (areas 26 and 30) but a 100% agreement on performing CPR (areas 1 and 2). However, there is a clear distinction in the results, where the abilities to assess and identify specific diseases (area 49), to identify the causes of and the prevention of burns (area 50), and to assess and take care of sports injuries (area 51) were all identified as competencies that are not needed.
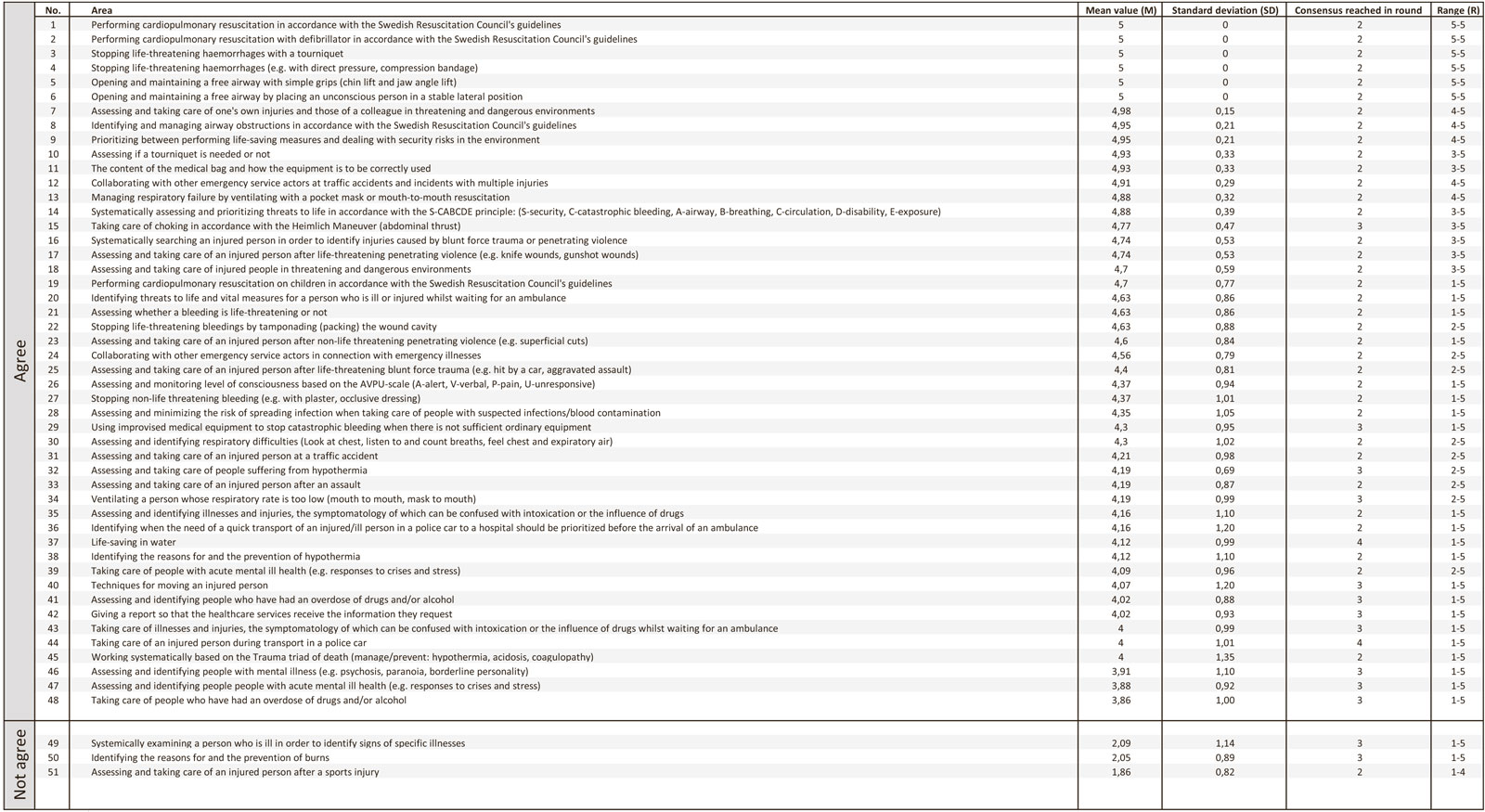
Table 3
Overview on areas reaching consensus regarding necessary emergency competencies.
4. Discussion
The procedure of selecting the participants, which is a core part of Delphi studies, followed an ongoing critical review among all the authors of the selection of experts (Wakefield & Watson, 2014). The expert group was homogeneous in relation to the focus of the study and heterogeneous in terms of its variation of backgrounds as educators, instructors, or PPOs. A potential limitation is that there may be gatekeepers in the organizations who identified the experts, and there may thus be experts who are not included in the study. On the other hand, the ambition in the Delphi process of selecting a group of highly trained and competent experts within the specialized field of knowledge related to the target issue is considered as a strength of the study (Hsu & Sandford, 2007). All the eligible experts from the currently available cohort of active experts in the subgroups of instructors and educators were included. In order to strengthen the empirical perspective on the data, the subgroup of PPOs with direct experience of the practical field and who represented all the police regions in Sweden were the largest group of the experts. The size of the group of experts (n=43) correlates with the sizes referred to in the literature (Hsu & Sandford, 2007). However, consensus concerning the optimal number of experts in a Delphi study has not been achieved in the literature, with variations from approximately 10 to several hundred (Keeney, Hasson & McKenna, 2011; Powell, 2003). Having a small number of experts can entail a risk that the outcome of the study is not representative. On the other hand, a larger number of participants could entail a risk of a lower response rate. The 100% response rate throughout all four rounds is considered to be a strength.
The experts were encouraged in Round 1 to define in free text what a Swedish PPO needs to know in order to help acutely ill or injured people. The use of free-text answers in Round 1 can be seen as a strength as it provides the participant with the opportunity of reflecting upon and answering a question without being influenced by an interviewer. Interviews can provide the possibility of posing follow-up questions in order to gain clarity and interpretation of the answers, and the researcher retains some influence over the generation of data. This, on the other hand, should be decreased in order to maintain an inductive approach (Wakefield & Watson, 2014). In order to reinforce the results from Round 1 and reduce the risk of bias due to the composition of the questionnaire, the free-text answers were subjected to a test of their face validity by a group of five clinically experienced PPOs and police program educators. The data collected in Round 1 was considered to be rich as it resulted in 76 necessary emergency care competence areas.
The 75% consensus cut-off point was predetermined and arbitrary. However, the percentage, which was considered to be reasonable by the authors, was supported by the literature (Keeney et al., 2011; Hsu & Sandford, 2007) and relevant for the aim of the study. This predetermined consensus rate could benefit and strengthen the outcome of the study in the ambition of exploring areas of competence in emergency care among PPOs. On the other hand, a lower consensus cut-off rate would have led to a larger number of areas with consensus.
The study results reveal three domains, containing several related areas of necessary emergency care competence for Swedish PPOs: (i) Performing basic life support measures preferably in a CPR situation or when encountering traumatic injuries, (ii) Assessments and measures for acutely ill people, and (iii) Initiating care responses for people with mental illness. The results also indicate a consensus regarding lower levels of agreement, for example, for the assessments concerning respirations/consciousness, identification, and evaluation of threats to life. These assessments form the basis for making a decision about which measures are to be applied in situations that concern life threats, which had in themselves received high levels of agreement (e.g., CPR, haemorrhage control measures). These potentially equivocal results could be interpreted as being difficult, possibly indicating ambiguities among the experts concerning the PPOs first responder role, responsibilities, needed emergency care training, and competence.
The PPOs are seen worldwide as a key component in the out-of-hospital chain of survival by sometimes being first on the scene, performing lifesaving interventions whilst awaiting ambulance service arrival (Klassen et al., 2018: Hollenberg et al., 2009; Husain & Eisenberg, 2013; Krammel et al., 2020). The results of this study indicate the highest level of consensus in terms of areas related to actions where the PPOs perform basic life support measures, with the two areas with the highest level of agreement linked to the ability of performing CPR. This could be due to the PPOs in Sweden, more often in urban areas, being dispatched as the first responders to out-of-hospital cardiac arrests (OHCA), where they then await the arrival of the ambulance service (Hollenberg et al., 2009). This intervention has shown to be successful in terms of the PPOs’ ability to ensure a quick response and to start CPR, which has led to an increased rate of OHCA survival (Husain & Eisenberg, 2013). Moreover, areas where PPOs perform lifesaving interventions on people suffering from a trauma have a high level of agreement. This may indicate that the PPOs often encounter situations where people are exposed to traumas, and, by being ambulatory, they can ensure a quick response. As in OHCA situations, a quick response to a trauma is crucial (Blackwell & Kaufman, 2002), especially in situations where a person suffers from a massive hemorrhage (Kragh et al., 2009). However, being first on the scene, encountering a person suffering from acute illness or injuries and making decisions as a PPO prior to the arrival of the ambulance service, is described as stressful (Hasselqvist-Ax et al., 2019; Backteman-Erlanson et al., 2011). PPOs state that they have great expectations from society concerning managing emergency care as first responders on the scene of an accident (Elmqvist et al., 2010), where a lack of appropriate emergency care training is mainly expressed as a cause of the stress (Hasselqvist-Ax et al., 2019). However, training in a systematic way of assessing and applying measures to acutely ill and injured persons creates the prerequisites for feelings of security as a first responder (Elmqvist et al., 2010) and may improve the outcome for the persons in need of care (PHTLS, 2020).
Despite consensus being achieved regarding the ability to assess and take care of acutely ill people, these areas had a lower level of agreement. In addition, consensus was not achieved for areas concerning competence in identifying or assessing specific diseases necessary for PPOs emergency care competence, and little is known about which type of medical emergencies Swedish PPOs respond to. Three British studies (Payne-James et al., 2010; McKinnon & Grubin, 2012; Miles et al., 2020) focusing on healthcare problems for detainees in police custody reveal that, despite containing a fairly young population (≈ 40 years), nearly 40% of the detainees had previous significant medical conditions, of whom more than one third had previous significant surgical conditions (Payne-James et al., 2007). Similar results were shown by McKinnon & Grubin (2013), where one fourth of all detainees under custody suffered from abdominal symptoms, and 19% had cardiovascular complaints over the past month. In addition, 16% of detainees suffered from asthma, 5% from diabetes and 2% from epilepsy (McKinnon & Grubin, 2013). Moreover, the main reason for referral from custody to hospital for medical problems was chest pains and diabetic ketoacidosis (Miles et al., 2020). These research findings may also be critically reflected upon in the light of Swedish legislation (FAP 023-1) regarding the fact that PPOs are assigned to people whose consciousness is affected by suspected drug or alcohol use. The Swedish PPOs dealt with approximately 50–60,000 assignments annually related to suspected drug or alcohol use during the years 2018–2020 (5–6% of all registered incidents) (Polisen.se, 2020). PPOs are, according to the aforementioned legislation (FAP 023-1), directed to decide whether the person should be taken to police custody or taken to the hospital for a medical examination. This may be seen as a qualified medical assessment, and great responsibility is, thus, placed on the PPOs’ emergency care competence in assessment and decision-making.
The results further indicate consensus regarding assessing and taking care of people with mental illness, although there was a low level of agreement about this competence. However, research studies from other countries show that the most common primary diagnosis for patient transport to emergency departments by PPOs is often mental illness (Crilly et al., 2019; Rosen & Travelers, 2021). Mental illness can be seen as a spectrum that includes both severe disorders/diseases and common mental health problems and/or mild symptoms of distress; examples include schizophrenia, anxiety, bipolar disorder, substance use disorder, depression, self-harm, sleeping difficulties, and distress (Bremberg & Dalman, 2015). Mental illness is a global public health problem (WHO, 2017; WHO, 2013), and people with mental illness are a significant group encountered in police work. The police in Sweden registered approximately 52,000 incident reports in 2019 (5% of the total of incident reports in 2019) where the PPOs encounter people with mental illness (Polisen.se, 2021a) and in 2020, an average of 60 calls per day were received by the police command centers, which deal with people who do not want to live any longer (Polisen.se, 2021b). Mental illness is also a common feature, for example, in fatal violence within the family (Brå, 2019). The need for PPOs to improve their competence in encountering people with mental illness is not a new demand (Meehan, 1995) and neither is the PPOs experience of frustration when they encounter people with mental illness that need care and do not receive it (McNiel et al., 1991). The results should be viewed in the light of encountering people with mental illness being a part of the PPOs’ everyday work, where each encounter is unique (Brink et al., 2011). The encounter requires competence in assessing the situation, for example, occurrence of suicide risk, danger, and the need for care. The PPOs need to make decisions about how to best respond in the encounter (Watsona et al., 2014). In order to succeed in this, the PPOs need the capability to approach the person with both comfort and respect in addition to having greater knowledge (Soares & Costa, 2019). There are several examples of co-responder models that support PPOs in their encounters with people with mental health care needs in the US, Australia, the UK, and Canada, e.g., phone support, extended educational support, or by a police-mental health co-responder team. The co-response models were associated with a reduction in the use of police powers of detention and a reduction in detainment in police custody (Puntis et al., 2018). The use of PAM (Psychiatric Acute Mobility) ambulances in mostly urban areas is increasing in Sweden to meet the growing needs of people with mental health problems (Lindström et al., 2020). However, both Lindström et. al. (2020) and Puntis, et. al. (2018) conclude that there is a need for more research to evaluate the outcomes of co-response models. In the light of the international initiatives to address the growing needs of people with mental health problems (WHO, 2019), it is, thus, somewhat surprising that the level of agreement for assessing and caring for people with mental illness was low in the present study findings. The reasons for this are not evident and have not been focused on. However, the distinction between emergency care and mental health care in the syllabus and police training could possibly contribute to an explanation. This is unfortunate since more than 50,000 assignments a year, which corresponds to approximately 5% of the daily workload of Swedish PPOs, require a competence in the assessment and care of people with mental ill health for identifying their individual needs.
4.3 Limitations
The study results should be viewed in light of the fact that the experts’ individual perspective on the study aim may have varied whilst participating in the study. One perspective might be to address the research question based on personal knowledge and experiences of what a PPO actually needs to know in relation to the empirical challenges to be encountered in the field. Another perspective might be that the answers are based on opinions about which societal role and scope of practice the expert finds relevant for PPOs. However, the information that was sent out to the experts clarified that the research question should be addressed, and their response given, based on their personal expertise of what a PPO actually needs to know in order to deal with the challenges to be encountered in their everyday police work.
5. Conclusions and implications
Swedish PPOs are expected to deal with a wide range of situations demanding acute assessments, measures, and decisions regarding people suffering from mental health problems, traumatic injuries, and medical illnesses. Educators at the police programs and instructors in the Swedish Police Authority need to acknowledge and support PPOs with emergency care training that corresponds to the responsibility Swedish legislation and their everyday police work places on them. The detailed presentation of necessary emergency care competence in the study may inform all stakeholders in the educational planning and execution of emergency care training for PPOs. The identified competence should be supported during the police programme training and followed up with an annual mandatory training to support the PPOs’ ability to cope with emergency care situations. The present study primarily systematizes the wealth of experience originating from the experts’ combined theoretical education and practical training. It could be said that the results mirror proven experience in this field. However, the education of professionals (PPOs included) is to be explicitly founded on proven experience and science. We hope that researchers can obtain empirical material in subsequent studies which more objectively highlights the practical expectations on PPOs. Close collaboration with the Police Authority is an essential element for attaining this. A development of the index codes for emergency care incidents in the Swedish police assignment databases needs to be initiated in order to obtain more detailed and complete data for analysis. Otherwise, researchers may have difficulties in coping successfully with the data analysis. Various co-response models and educational interventions should be further developed and researched in order to support PPOs and people with mental health care needs.
Acknowledgement
We acknowledge and appreciate all experts who participated in our study.
References
-
Alonso-Serra, H. M.,Delbridge, T. R.,Auble, T. E.,Mosesso, V. N., &Davis, E. A.(1997). Law Enforcement Agencies and Out-of-Hospital Emergency Care.
Annals of Emergency Medicine
, 29(4), 497-503. https://doi.org/10.1016/S0196-0644(97)70223-3 -
Backteman-Erlanson, S.,Jacobsson, A.,Öster, I., &Brulin, C.Caring for Traffic Accident Victims: The Stories of Nine Male Police Officers.
International Emergency Nursing
. 19.2 (2011): 90-95. https://doi-org.proxy.lnu.se/10.1016/j.ienj.2010.06.001 -
Band, R. A.,Salhi, R. A.,Holena, D. N.,Powell, E.,Branas, C. C., &Carr, B. G.(2014). Severity-adjusted mortality in trauma patients transported by police.
Annals of emergency medicine
, 63(5), 608–614.e3. https://doi.org/10.1016/j.annemergmed.2013.11.008 -
Blackwell, T. H., &Kaufman, J. S.(2002). Response time effectiveness: comparison of response time and survival in an urban emergency medical services system.
Academic emergency medicine : official journal of the Society for Academic Emergency Medicine
, 9(4), 288–295. https://doi.org/10.1111/j.1553-2712.2002.tb01321.x -
Bremberg, S.&Dalman, C.(2015).
Begrepp, mätmetoder och förekomst av psykisk ohälsa och psykiatriska tillstånd hos barn och unga. En kunskapsöversikt
.Forte
. -
Brink, J.,Livingston, J.,Desmarais, S.,Greaves, C.,Maxwell, V.,Michalak, E.,Parent, R.,Verdun-Jones, S., &Weaver, C.(2011).
A study of how people with mental illness perceive and interact with the police
.Mental Health Commission of Canada
. Retrieved from http://www.mentalhealthcommission.ca -
Brottsförebyggande rådet (Brå) (2019).
Dödligt våld i Sverige 1990–2017. Omfattning, utveckling och karaktär
. Rapport 2019:6.Brottsförebyggande rådet
. https://www.bra.se/publikationer/arkiv/publikationer/2019-06-04-dodligt-vald-i-sverige-1990-2017.html -
Crilly, J.,Zhang, P.,Lincoln, C.,Scuffham, P.,Timms, J.,Becker, K.,van Buuren, N.,Fisher, A.,Murphy, D., &Green, D.(2019). Characteristics and outcomes of patient presentations made by police to an Australian emergency department.
Emergency medicine Australasia : EMA
, 31(6), 1014–1023. https://doi.org/10.1111/1742-6723.13301 -
Dekanoidze, K.,Khelashvili, M.(2018).
Police education and training systems in the OSCE region
. https://www.osce.org/project-coordinator-in-ukraine/423401 -
Elmqvist, C.,Brunt, D.,Fridlund, B., &Ekebergh, M.(2010). Being first on the scene of an accident–experiences of ’doing’ prehospital emergency care.
Scandinavian journal of caring sciences
, 24(2), 266–273. https://doi.org/10.1111/j.1471-6712.2009.00716.x -
Eraut, M.(1998). Concepts of competence.
Journal of Interprofessional Care
, 12(2), 127-139. https://doi-org.proxy.lnu.se/10.3109/13561829809014100 -
Erdner, A., &Piskator, R.(2013). Police experiences of committing people with mental illness to a hospital.
Issues Ment Health Nurs
, 34(7), 550-555. https://doi.org/10.3109/01612840.2013.783658 -
Hasselqvist-Ax, I.,Nordberg, P.,Svensson, L.,Hollenberg, J., &Joelsson-Alm, E.(2019). Experiences among firefighters and police officers of responding to out-of-hospital cardiac arrest in a dual dispatch program in Sweden: an interview study.
BMJ open
, 9(11), e030895. https://doi.org/10.1136/bmjopen-2019-030895 -
Hawkins, S. C.,Shapiro, A. H.,Sever, A. E.,Delbridge, T. R., &Mosesso, V. N.(2007). The role of law enforcement agencies in out-of-hospital emergency care.
Resuscitation
, 72(3), 386–393. https://doi.org/10.1016/j.resuscitation.2006.07.021 -
Hollenberg, J.,Riva, G.,Bohm, K.,Nordberg, P.,Larsen, R.,Herlitz, J.,Pettersson, H.,Rosenqvist, M., &Svensson, L.(2009). Dual dispatch early defibrillation in out-of-hospital cardiac arrest: the SALSA-pilot.
European heart journal
, 30(14), 1781–1789. https://doi.org/10.1093/eurheartj/ehp177 -
Hsu, C.andSandford, B.(2007) The Delphi Technique: Making Sense of Consensus.
Practical Assessment, Research & Evaluation
, 12, 1-8. http://pareonline.net/pdf/v12n10.pdf -
Husain, S., &Eisenberg, M.(2013). Police AED programs: a systematic review and meta-analysis.
Resuscitation
, 84(9), 1184–1191. https://doi.org/10.1016/j.resuscitation.2013.03.040 -
Keeney, S.,Hasson, F., &McKenna, H.(2011).
The delphi technique in nursing and health research
.West Sussex
:Wiley and Blackwell
. ISBN:978-1-405-18754-1
-
Klassen, A. B.,Core, S. B.,Lohse, C. M., &Sztajnkrycer, M. D.(2018). A Descriptive Analysis of Care Provided by Law Enforcement Prior to EMS Arrival in the United States.
Prehospital and disaster medicine
, 33(2), 165–170. https://doi.org/10.1017/S1049023X18000213 -
Kooij, F. O.,van Alem, A. P.,Koster, R. W., &de Vos, R.(2004). Training of police officers as first responders with an automated external defibrillator.
Resuscitation
, 63(1), 33–41. https://doi.org/10.1016/j.resuscitation.2004.03.015 -
Kragh, J. F., Jr,Walters, T. J.,Baer, D. G.,Fox, C. J.,Wade, C. E.,Salinas, J., &Holcomb, J. B.(2009). Survival with emergency tourniquet use to stop bleeding in major limb trauma.
Annals of surgery
, 249(1), 1–7. https://doi.org/10.1097/SLA.0b013e31818842ba -
Krammel M,Lobmeyr E,Sulzgruber P,Winnisch M,Weidenauer D,Poppe M, et al. (2020) The impact of a high-quality basic life support police-based first responder system on outcome after out-of-hospital cardiac arrest.
PLoS One
15 (6): e0233966. https://doi.org/10.1371/journal.pone.0233966 -
Lindström, V,Sturesson, L,Carlborg, A.Patients’ experiences of the caring encounter with the psychiatric emergency response team in the emergency medical service—A qualitative interview study.
Health Expect
. 2020; 23: 442–449. https://doi.org/10.1111/hex.13024 -
Meehan, A. J.(1995). From conversion to coercion: the police role in medication compliance.
The Psychiatric quarterly
, 66(2), 163–184. https://doi.org/10.1007/BF02238862 -
McKinnon, I. G., &Grubin, D.(2013). Health screening of people in police custody–evaluation of current police screening procedures in London, UK.
European journal of public health
, 23(3), 399–405. https://doi.org/10.1093/eurpub/cks027 -
McNiel, D. E.,Hatcher, C.,Zeiner, H.,Wolfe, H. L., &Myers, R. S.(1991). Characteristics of persons referred by police to the psychiatric emergency room.
Hospital & community psychiatry
, 42(4), 425–427. https://doi.org/10.1176/ps.42.4.425 -
Miles, T.,Webb, V.,Kevern, P.,Shibchurn, R.,Bird, T., &Finch, G.(2020). Custody early warning scores; Do they predict patient deterioration in police custody?.
Journal of forensic and legal medicine
, 76, 102069. https://doi.org/10.1016/j.jflm.2020.102069 -
National Swedish police authority (2020)
Utbildningsplan för Polisprogram
. A070.568/2018.Stockholm
:Polismyndigheten
. -
Payne-James, J.J.,Green, P.G.,Green, N.,McLachlan, G.M.C,Munro, M.H.W.M.andMoore, T.C.B.Healthcare Issues of Detainees in Police Custody in London, UK.
Journal of Forensic and Legal Medicine
17.1 (2007): 11-17. https://doi-org.proxy.lnu.se/10.1016/j.jflm.2007.10.011 -
PHTLS: Prehospital Trauma Life Support for First Responders, 9th Edition (online access included). (2020).
ProtoView
, 2020(28), ProtoView, 2020-07-14, Vol.2020 (28). -
PMFS 2016:9. (FAP 776:1).
Polismyndighetens föreskrifter om Polismyndighetens föreskrifter och allmänna råd om utbildning i polisiär konflikthantering
. https://polisen.se/lagar-och-regler/polismyndighetens-forfattningssamling/ -
Polisen.se (2020).
Polismyndighetens årsredovisning 2020. Polismyndigheten
. Retrived 211213. https://polisen.se/aktuellt/nyheter/2021/februari/arsredovisning-2020-starkt-fortroende-och-forbattrat-utredningsresultat/ -
Polisen.se. (2021a).
Ökad kompetens inom psykisk ohälsa och suicid
. Retrived 210501. https://polisen.se/aktuellt/nyheter/2020/maj/okad-kompetens-inom-psykisk-ohalsa-och-suicid/ -
Polisen.se. (2021b).
Psykisk ohälsa en stor del av polisens uppdrag
. Retrived 210501. https://polisen.se/aktuellt/nyheter/2021/februari/psykisk-ohalsa–en-stor-del-av-polisens-uppdrag/ -
Powell C. (2003). The Delphi technique: myths and realities.
Journal of advanced nursing
, 41(4), 376–382. https://doi.org/10.1046/j.1365-2648.2003.02537.x -
Puntis, S.,Perfect, D.,Kirubarajan, A,Bolton, S.,Davies, F.,Hayes, A.,Harris, E., &Molodynski, A.A systematic review of co-responder models of police mental health ‘street’ triage.
BMC Psychiatry
18, 256 (2018). https://doi.org/10.1186/s12888-018-1836-2 -
Rosen, D. L., &Travers, D.(2021). Emergency department visits among patients transported by law enforcement officers.
PloS One
, 16(1), e0244679. https://doi.org/10.1371/journal.pone.0244679 -
RPSFS 2000:57. (FAP 023-1).
Rikspolisstyrelsens föreskrifter och allmänna råd om omhändertagande av berusade personer
. https://polisen.se/lagar-och-regler/polismyndighetens-forfattningssamling/ -
Soares, R., &Pinto da Costa, M.(2019). Experiences and Perceptions of Police Officers Concerning Their Interactions With People With Serious Mental Disorders for Compulsory Treatment.
Frontiers in psychiatry
, 10, 187. https://doi.org/10.3389/fpsyt.2019.00187 -
SOU 2008:39.
Framtidens polisutbildning
. https://www.regeringen.se/rattsliga-dokument/statens-offentliga-utredningar/2008/04/sou-200839/ -
SOU 2016:39.
Polis i framtiden – polisutbildningen som högskoleutbildning
. https://www.regeringen.se/rattsliga-dokument/statens-offentliga-utredningar/2016/05/sou-201639/ -
Sztajnkrycer, M. D.,Callaway, D. W., &Baez, A. A.(2007). Police officer response to the injured officer: a survey-based analysis of medical care decisions.
Prehospital and disaster medicine
, 22(4), 335–342. https://doi.org/10.1017/s1049023x00004970 -
Wakefield, R., &Watson, T.(2014). A reappraisal of Delphi 2.0 for public relations research.
Public Relations Review
, 40(3), 577–584. https://doi.org/10.1016/j.pubrev.2013.12.004 -
Watson, A. C.,Swartz, J.,Bohrman, C.,Kriegel, L. S., &Draine, J.(2014). Understanding how police officers think about mental/emotional disturbance calls.
International journal of law and psychiatry
, 37(4), 351–358. https://doi.org/10.1016/j.ijlp.2014.02.005 -
World Health Organization (WHO). (2013). World Health Organization.
Mental health action plan 2013–2020
.Geneva
. https://www.who.int/publications/i/item/9789241506021 -
World Health Organization (WHO). (2017).
World health statistics 2017: monitoring health for the SDGs, sustainable development goals
.Geneva
. https://apps.who.int/iris/handle/10665/255336 -
World Health Organization (WHO). (2019).
The WHO special initiative for mental health (2019-2023): universal health coverage for mental health
.World Health Organization
. https://apps.who.int/iris/handle/10665/310981. License: CC BY-NC-SA 3.0 IGO
- 1International standard for first responders acting in emergency care situations: S = Safety, C = Critical hemorrhage, A = Airway, B = Breathing, C = Circulation, D = Disability, E = Exposure (PHTLS, 2020).